Pain is how our nervous system senses real or potential damage. It is a warning signal that alerts the body to avoid further harm. Understanding pain is key to fixing it. There are many types of pain with many different root causes. Read on to discover how pain works and how to mitigate it.
What is Pain?
The International Association for the Study of Pain defines pain as “an unpleasant sensory and emotional experience that is associated with actual or potential tissue damage.” It serves as the body’s protective withdrawal mechanism or warning signal both from physical damage and to allow for healing to occur. Through a learned process, an individual may avoid similar situations in the future that may cause pain [1].
Interestingly, the level of pain might not always correspond to injuries or tissue damage to the body [2]. Many people have pain with no detectable injuries, while some people have a lot of physical damage with no pain.
Simple painkillers and pain relief medications for acute pain provide effective results 20 – 70% of the time. However, oral painkillers are not effective at reducing the duration of chronic pain [3].
Identifying pain based on its location, duration, and intensity can point to the underlying causes as well as the most effective treatments [4].
Acute vs. Chronic Pain
Acute pain is a normal response to harmful stimuli, injuries, or a disease. Typically, this pain resolves once the stimuli are removed, or the damaged tissue is healed or relatively soon thereafter [5].
Acute pain stimuli also activate the fight-or-flight mechanisms and may cause muscle spasms [6].
Acute pain is experienced immediately and can potentially last up to 3 months. Pain that lasts more than 3 months after the injury is categorized as chronic pain [7].
Chronic pain is due to persistent activation of nociceptors (neurons that help transmit pain signals to the brain) in the areas around the damaged tissue. However, chronic pain may continue despite any identifiable triggers, damage, or injury.
Common chronic pain disorders include [5]:
- Chronic low back pain
- Headaches
- Myofascial pain syndrome
- Fibromyalgia
- Neuropathic pain
- Phantom limb pain
- Central pain syndrome: a brain condition caused by damage to or dysfunction of the nervous system [8].
Abnormalities in the nervous system can result in lasting pain long after the original injuries have disappeared, as is the case of complex regional pain syndrome [9]. Symptoms include swelling, changes in muscle tone, immobility, and reduction in blood flow to the affected area.
Independent of the cause, chronic pain results from a sustained sensory abnormality in the body.
Chronic pain is a result of many factors, including overall health, psychological factors, and hormones [10].
Uncontrolled chronic pain can decrease immune function, promote tumor growth, and hinder the healing process, increasing the risk of disease (morbidity) [11].
Mechanisms of Action for Physical Pain
There are three types of physical pain with distinct mechanisms of action. Each type requires different treatments to relieve or eliminate it [12].
1) Harmful Stimuli
Nociceptors are specialized pain-sensing receptors on the skin and limbs [13]. Nociceptive pain is caused by extreme temperatures, pressure, or chemicals [13].
While nociception is a sensation, the feeling of pain is a perception. If certain nerves or receptors are blocked, there will be nociception without pain [14].
The signal created by the activation of nociceptors is proportional to the strength of the stimulus or degree of damage [15].
When the stimulus intensity reaches a point called the noxious threshold, nociceptors are activated [16].
The axons involved with nociception are relatively slow to conduct pain signals to the brain. These axons are typically lightly myelinated (insulated to increase action potential conduction and speed up nerve signals) or more commonly unmyelinated [17].
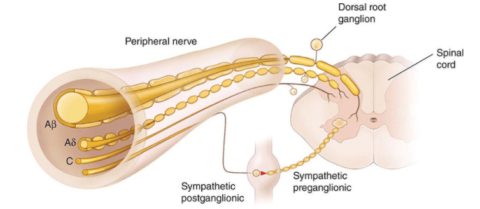
These types of axons are present in the two major classes of pain neurons. The first class has medium-diameter and myelinated axons that transmit acute, well-localized fast pain. The second class of nociceptors is small unmyelinated “C” fibers that transmit poorly localized slow pain [16]. The pain signal travels to the brain (cerebral cortex), where the signal is processed.
Although most nociceptors are located in the skin, some nociceptors are found in internal organs such as the heart, lungs, testes, and the digestive tract [18].
2) Inflammation
In inflammatory pain, inflammatory proteins released by white blood cells (IL-1β, IL-6, TNF-α, IL-12, IL-18, IFNγ) activate the nociceptors, rather than damaging stimuli such as heat or pressure [15, 19, 20].
In addition to these inflammatory proteins, the following substances also sensitize the nociceptors in the damaged tissue [21]:
- Potassium, prostaglandins, and leukotrienes released by damaged cells
- Serotonin released by platelets
- Bradykinin released in the blood
- Histamine released by mast cells
- Substance P released by primary afferent nerve fibers
These substances expand blood vessels (vasodilation) and increase swelling in the damaged tissues [22].
Inflammatory pain is meant to protect an injured body part and promote healing and rest [23].
The skin, joints, and gut are susceptible to inflammatory pain, which can appear as inflammation of the skin (such as atopic dermatitis), arthritis, and inflammatory bowel disease [24].
3) Inflammation in the Brain (Pathological Pain)
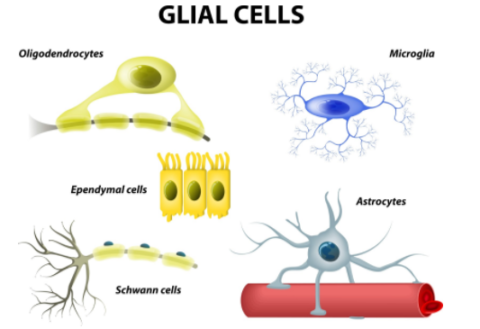
In pathological pain, inflammation in the brain causes brain dysfunction. Neurons and immune cells in the brain (astrocytes and microglia) communicate with each other through inflammatory signals, which drive pain perception [25].
This leads to :
- pain perception in the absence of injuries or damaging stimuli
- increased pain sensitivity
- exaggerated pain in response to harmless stimuli
Unlike nociceptive and inflammatory pain, pathological has no protective purpose [23, 25]. In addition, it does not travel along the traditional pain pathways [26].
Causes of Pathological Pain
- Severe trauma [27]
- Stress [27]
- Brain diseases that reorganize brain connections, which alters the pain pathway [26]
- The incongruence between body positioning (proprioception), movement, and intentions may lead to pathologic pain and nausea, such as in the case of motion sickness [28]
Examples of Pathologic Pain
Medical conditions with pathologic pain as a symptom include [23]:
- Fibromyalgia: widespread muscle pain and tenderness
- Irritable bowel syndrome: a chronic gut condition characterized by stomach pain, gas, and bloating
- Tension-type headaches: the band-like pain of mild to moderate intensity in the head, scalp, or neck
- Temporomandibular joint disease: pain and immobility of the jaw and surrounding muscles
- Interstitial cystitis: persisting discomfort or pain in the urinary bladder and pelvic region
- Phantom limb pain may be a pathologic pain. It is common among amputees. Although the brain no longer receives signals from a lost body part, these individuals still feel neuropathic pain [29].
4) Neuropathic
Neuropathic pain is caused by nerve damage that may be inside or outside the brain. This damage leads to changes in pain processing, which can cause pain or increased pain sensitivity [30, 31].
Two types of neuropathic pain are hyperalgesia and allodynia, which may coexist in the same patient [32].
Hyperalgesia is when nerve damage enhances pain sensitivity in the region [21].
Allodynia occurs when harmless stimuli that ordinarily would not cause pain is perceived as painful.
5) Psychogenic
Psychogenic pain does not have a physical cause because it is not associated with a diagnosed disease. Causes can be emotional or mental stressors, psychological disorders, or psychiatric disorders [33].
It is hard to distinguish between the physical and psychogenic origin of pain. In addition, someone may be experiencing both physical and psychogenic which may not be related [34].
There are a few significant differences between symptoms of psychogenic vs. physical pain. According to one study, patients with psychogenic pain tend to report higher bodily discomfort but less cognitive dysfunction than patients with physical pain [35].
The mechanism of action for psychogenic pain is not well understood. Further studies are needed to differentiate between psychogenic pain and sources of physical pain [36].
However, strong familial and social support can help with psychogenic pain by helping to cope with the stress associated with the pain [37].
Measuring Pain Intensity
Pain intensity is subjective and difficult to gauge in patients [38].
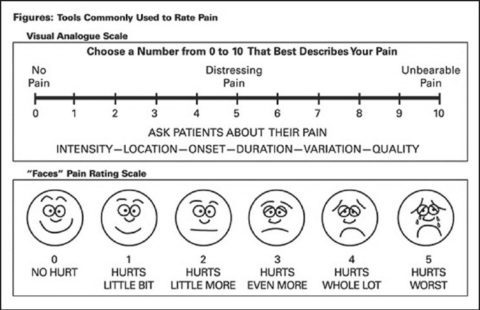
There are four scales used to measure pain intensity in an individual, including [39]:
- The Visual Analogue Scale consists of a straight line spectrum with endpoints of “no pain” to the “worst pain possible.” The rating is based on the subjectivity of the patients, marking the degree of their pain on the straight line [40].
- The Numerical Rating Scale asks patients to rate their current pain on a scale from 0 (“no pain”) to 10 (“worst possible pain”) [41].
- Verbal Rating Scale consists of a series of adjectives reflecting degrees of pain severity. These words are arranged from “no pain” to the most pain perceivable [42].
- For the Faces Pain Scale-Revised, the faces of the patients are matched to the faces of the scale to determine pain intensity levels [43, 44].
Surprising Factors that May Worsen Pain
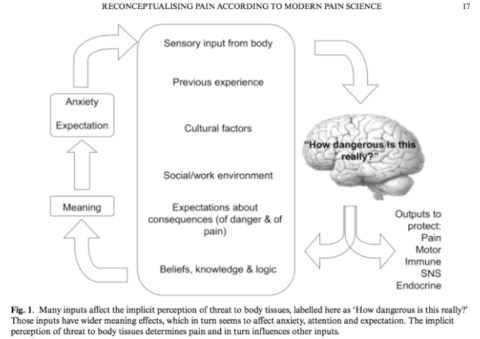
Based on modern pain science, we now know that the presence of pain and pain severity generally does not reflect tissue damage. Rather, the pain is how our brain powerfully tells us to protect our tissues. The longer the pain lasts, the less the pain indicates the degree of tissue damage.
The following factors can make pain worse, regardless of the type of pain [45]:
- Increased inflammation, by increasing nociceptor activity
- Increased temperature, by increasing nociceptor activity
- Decreased blood flow to the area where pain originates increases nociceptor activity by increasing acidity in the area
- Thoughts and attention can increase pain
- Stress, depression, and anxiety may increase pain [46]
Also, threat perception increases pain.
- Environmental cues for danger, which make you think that the damaging stimuli are more harmful than they actually are. Conversely, cues that signal that the pain will be relieved, such as the use of pain medications (placebo effect).
- Catastrophic interpretation of the pain makes pain worse.
- Believing that the pain is an accurate indicator of damage makes pain worse while believing the opposite reduces the pain.
- Social and religious contexts. For example, people may feel less pain when they self-inflict pain during religious rituals.
- Overactivation of the nervous system may increase the pain.
- Hormones: Estrogen has a pain-suppressing effect [47]. Women often feel more pain when their estrogen levels are low [48].
Chronic Pain
Pain is a symptom of many diseases and syndromes. These include but are not limited to:
- Cancer: One of the most feared symptoms of cancer is pain. Pain management in cancer patients is a continuous and challenging issue [49].
- Fibromyalgia is a common chronic disorder characterized by widespread pain and tenderness in the muscles [50].
- Migraines are characterized as severe, complex pain on one or both sides of the head [51].
- Myofascial Pain Syndrome originates in the muscles (myofascial trigger points) [52].
- Osteoarthritis: The breakdown of joint cartilage leads to pain, stiffness, and immobility [53].
9 Natural Ways to Manage Pain
Pain management is a complex medical field. If you are experiencing unexplained pain, talk to your doctor for an accurate diagnosis of any underlying conditions.
1) Managing Inflammation
Your doctor can help you determine appropriate steps to take to manage any uncontrolled inflammation.
If you suspect that some of your inflammation comes from foods, your doctor or nutritionist may recommend an elimination diet to identify potential triggers. Lack of sleep, altered circadian rhythm, autoimmunity, and chronic stress can also be sources of inflammation.
2) Cold Exposure and Ice
Cold showers can help reduce inflammation overall, while icing the injuries can temporarily reduce pain. In addition, cold exposure may trigger endorphin release [54, 55].
3) Stimulating Blood Flow
In cases of injuries that have already healed up or when there is no longer tissue damage, stimulating blood flow to the area may ease the pain.
Therapies that stimulate blood flow to the area include:
- Massage and other forms of manual therapies [56, 57]
- Cupping therapy
- Acupuncture
- Alternating hot/cold therapy
- Ultrasound therapy
- Infrared light therapy
Talk to your doctor before undergoing any of these therapies. If your pain is being caused by tissue damage, they may do more harm than good.
4) Psychotherapy
Thoughts and perception of threats may increase pain.
The following mental/emotional factors can affect pain [58, 59, 60]:
- Thoughts
- Emotions
- Social and familial support
- Cultural background
- Context and memory associated with the pain (through conditioning)
Cognitive behavioral therapy improved the overall quality of life in some individuals with chronic pain, with modest effectiveness [61].
Acceptance and commitment therapy focuses on the context of how the patients feel the pain [62]. Increasing the acceptance of the pain and the context can help reduce pain. This is most likely effective as a chronic pain management strategy [63].
Clinical hypnosis can reduce pain in adults and children, and has been observed to reduce acute pain, migraines, arthritic pain, cancer pain, and surgery pain [64, 65].
Managing Stress and Anxiety
The relationship between stress and pain is complex. In some people, stress makes pain worse. In others, it helps relieve the pain.
In many people with chronic pain, chronic stress usually makes the pain worse [66, 67].
Acute stress can relieve pain because cortisol and adrenaline are actually pain-relieving and anti-inflammatory hormones [68]. In addition, stress increases natural opioids in the brain [69].
Anxiety worsens pain through the hippocampus (memory center in the brain) [70]. In addition, chronic stress reduces serotonin levels and dopamine activity in the brain (nucleus accumbens) [71]. Chronic stress also reduces sensitivity to morphine (in rats), which means that stress affects the opioid system [72].
Stress-reduction approaches that may be effective for pain include [73]:
- Biofeedback training
- Deep breathing
- Progressive muscle relaxation
- Autogenic training (a relaxation technique)
- Visualization/guided imagery
- Therapies
These strategies may be appropriate for psychogenic pain or chronic pain. Talk to your doctor about whether they may help you.
5) Physiotherapy
Pain may not necessarily correlate with the degree of physical damage. However, poor movement patterns and imbalances may cause the body to reduce further harm to itself by causing pain [45].
Exercise and movements help ensure that injuries heal in a way that restores functional ability [74]. Lack of movements can reduce mobility and strength after the injuries heal.
Physical therapy involves [75, 76]:
- Exercise: For some patients, exercise can help manage pain. It strengthens bones and muscles, and improves mood, self-esteem, physical capacity, and decreases stress [77].
- Corrective movements, such as strengthening muscles around the injured areas, improving postures, and correcting poor movement patterns, can help reduce pain [78].
- Massage therapy reduced pain sensitivity at tender points by relaxing muscle tissues and also reduces stress by increasing oxytocin [56].
- Education and advice can help individuals understand their condition and make the best decisions addressing their issues [79].
- Mobility aids can assist in a patient’s balance and maintain motor functions [80].
Physiotherapy should be carefully overseen by a medical professional.
6) Supplements and Diet
Foods High in Calories, Fat, and Sugar can Alleviate Pain
Foods high in calories, fat, and sugar temporarily relieve pain by reducing stress and increasing serotonin. However, eating foods high in calories, fat, and sugar can lead to additional weight gain, which can increase inflammation, which may, in turn, cause greater pain and disability in the long term [81].
Foods high in fat and sugar that can provide temporary pain relief include:
- Mother’s milk alleviates acute and persistent pain in infants. However, this effect is only limited to pre-weaning infants. The exact reason for this exclusivity is still unknown [82, 83].
- Sugar: Emotional changes brought on by sugar consumption reduce pain caused by temperature and physical stressors and increase tolerance [84, 85].
- Fats can suppress physical allodynia and heat hyperalgesia [86].
- Soy and casein proteins can suppress heat hyperalgesia but not physical allodynia. The mechanisms are still unknown [86].
Supplements and Herbal Painkillers
The following substances have shown promise as painkillers in limited, low-quality clinical studies; there is currently insufficient evidence to support their use in this context, and they should never replace what your doctor prescribes. Remember to talk to your doctor before starting any new supplement or making significant changes to your diet.
Natural painkillers include [87]:
- Boswellia contains boswellic acid, which reduced inflammatory pain by lowering inflammation [88].
- Curcumin reduced sensitivity to pain, pain, and inflammation [89].
- MSM is a natural painkiller and anti-inflammatory agent. It reduced pain and swelling in the joints, increasing mobility [90, 91, 92].
- Cannabinoids (CBD/THC) bind to opioid and cannabinoid receptors, not only reducing inflammation but also releasing endorphins, which can reduce pain [93].
- Glucosamine is a natural component of cartilage and is used to reduce pain in osteoarthritis. This compound also blocked inflammation, reducing both pain and inflammation [94].
- D-phenylalanine is a synthetic amino acid that is believed to increase pain tolerance in the body by increasing a natural opioid called enkephalin in the brain, producing a mild and temporary reduction in pain [95, 96, 97].
Read this post to learn more about ways to relieve pain by increasing your body’s natural opioids.
8) Acupuncture
Acupuncture can alter pain signals to the brain by stimulating certain points (acupoints) in the body and triggering the release of pain-relieving neurochemicals such as endorphins, serotonin, and opioids in the brain [98, 99].
Acupuncture may not be appropriate for everyone. Talk to your doctor before trying it for the first time.
9) Transcutaneous Electrical Nerve Stimulation (TENS)
Transcutaneous electrical nerve stimulation (TENS) involves applying electrical current through electrodes placed on the skin to stimulate nerves and muscles, which can help reduce pain [100].
TENS helps with pain because stimulated electrical current travels faster than the pain signal, blocking the pain sensation. TENS is based on the gate-control theory of pain, where non-painful signals close the “gates” to pain signals [101].
TENS helps with rib fracture pain better than painkillers and may help with diabetic neuropathy [102].
However, TENS was not found to be effective against chronic low back pain, labor pain, or neck pain [103, 104, 105].
10) Caffeine
Caffeine can be used as a pain reliever or added to painkiller drugs to make the drugs more effective by [106, 107]:
- improving absorption of the painkillers into the body
- changing an individual’s perception of pain
- slowing the liver’s processing of drugs
Conventional Medical Treatments for Pain
Note: This section should not be construed as medical advice. Do not make any changes to your medication without consulting your doctor.
1) Medical Procedures
Interventional pain management includes medical procedures to treat pain using invasive techniques [108].
- Nerve blocks: anesthetics stop the flow of pain signals by blocking the nerve [109].
- Neurostimulation: electrical stimulation prevents and inhibits pain from reaching the nervous system [109].
- Anesthesia injections to local tissues will reduce pain along with physical sensations [109].
- Spinal cord stimulation: electrical stimulation of the dorsal horn of the spinal cord can relieve pain. However, the exact mechanisms of action are unknown [110].
Direct destruction of nervous tissues is now rarely used in pain treatment [111].
Interventional procedures are beneficial for patients who can’t go into surgeries for medical reasons and don’t respond well to medications. These therapies help with noncancer pains caused by dysfunction of the nervous system [112].
2) Painkiller Medications
Painkillers help with mild-to-moderate acute pain by treating the symptoms. These include Tylenol or nonsteroidal anti-inflammatory drugs (NSAIDs). Medication choice depends on the condition and risk factors of the patients. Some (cyclooxygenase-2 selective) NSAIDs can cause heart complications [113].
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Nonsteroidal anti-inflammatory drugs can reduce inflammation thus helping with pain. These drugs also reduce fever (antipyretic effects). These drugs include [114]:
- Aspirin
- Indomethacin
- Phenylbutazone
NSAIDs do have side effects, such as reducing the protective layers in the gut, which can cause stomach ulcers and intestinal permeability [115, 116]. In cases of injuries, actively reducing inflammation may prolong healing time [117].
Opioids
Opioids can help with severe acute and chronic pain. Opioids binding to opioid receptors reduce the sensation of pain in the brain and activate the reward pathway [118].
Opioid use can produce euphoric and pleasurable sensations but can lead to cravings and addiction [119, 120].
Overuse of opioids can lead to increased tolerance and hyperalgesia [118].
Opioid painkillers include [118]:
- Methadone (synthetic opioids)
- Fentanyl (synthetic opioids)
- Propoxyphene (synthetic opioids)
- Morphine (naturally synthesized)
- Codeine (naturally synthesized)
Paradoxically, opioid drugs used for anesthesia and pain relief sensitize the pain-sensing neurons [121]. This can make opioid users feel more pain when they are not using opioids.
Genes Associated with Pain Sensitivity
COMT controls opioid receptor activation and pain responses [122].
OPRM1 encodes a mu opioid receptor, which controls pressure pain [122].
OPRD1 encodes opioid receptor beta. The SNP Phe27Cys affects heat pain tolerance [122]. rs11988795 is associated with cold pain tolerance and responses [122].
GCH1 helps produce BH4, which is important in the production of several neurotransmitters [123]. This gene is associated with pressure pain, protecting against pain, and reducing hyperalgesia [122].
TRPV1 is a receptor that allows nociceptors to sense heat and cold. It is also a target of capsaicin [122, 124].
Other genes and SNPs potentially involved include:
- rs13361160 C allele (unknown gene) increases the risk of chronic widespread pain in joints [125].
- CD3E controls communication between T cells and is associated with inflammatory pain [126].
- MPZL2 is a protein on the cell surface that controls thymus and T-cell development. rs17122021 (no allele specified) is associated with more post-surgery pain [127].
- FTLP13 – rs2562456: This gene is an non-functional gene [128]. However, its SNP affects acute pain and the effectiveness of painkillers after oral surgery [129].